|
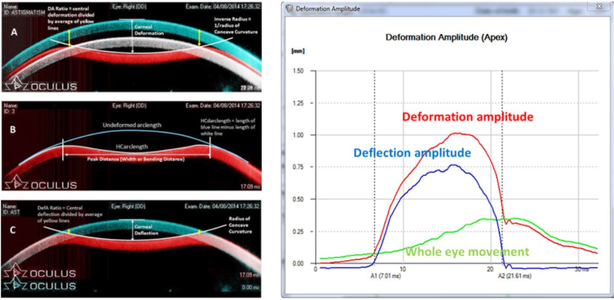
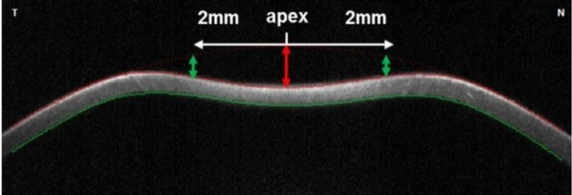
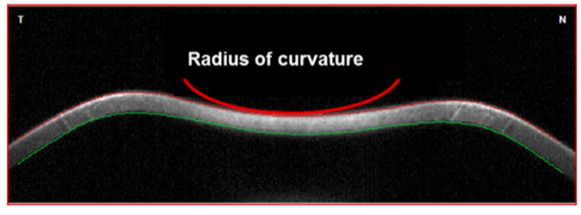
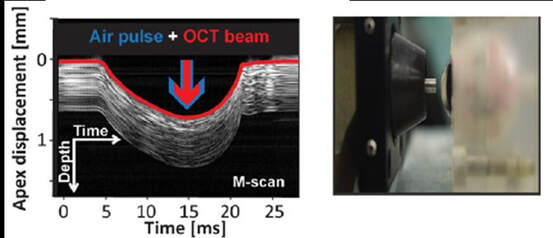
Sven Reisdorf, Product Manager at OCULUS The basic idea of the project device ImTopScanner is to derive information about the biomechanical properties from the OCT-based high-speed videos that monitor the corneal response to an air-pulse. Compared to the commercially already existing device based on Scheimpflug technology (Corvis ST) the OCT technology has the advantage to monitor the biomechanical response in different sectional planes. The following image illustrates the deformation response to the air pulse: At the beginning the cornea is in its initial convex shape. The air pulse drives the cornea backwards until the first applanation occurs when the cornea is flat and intraocular pressure (IOP) is determined. Afterwards, the cornea is further deformed until the moment of maximal concavity and then returns back to its original shape. Before it reaches the initial state, it passes through a second applanation, where the cornea is flat again. The images illustrate that one needs to distinguish between corneal movement and the movement of the whole eye as the whole globe moves slightly backwards (see image A). The red curve in the diagram illustrates the vertical displacement of the corneal vertex which is the sum of whole globe movement and corneal movement. By subtracting the movement of the whole globe from this curve one obtains the pure corneal movement (blue curve) which is the basis for further biomechanical analysis. Unfortunately, deriving biomechanical properties from the high-speed videos and these curves is not trivial as the movement of the cornea is not only influenced by the biomechanical properties but mainly by three factors: IOP, corneal thickness and biomechanical properties. A lot of knowledge in regards of the influence of these main factors on the deformation response has been gained by the Corvis ST and can now be applied to OCT technology. As corneal thickness can be measured easily the main task is to differentiate the influence of IOP and biomechanical properties. In order to achieve this goal, one needs to derive features from the images that are more dependent on IOP and features that are rather influenced by the biomechanical properties. These parameters can be used clinically directly for clinical applications such as keratoconus detection and as input parameters for machine learning(1). Even more important is that they can be used as input parameters for numerical simulations that can then derive very accurately the intrinsic material properties relatively independent on corneal thickness and IOP(3). Dynamic Corneal Response Parameters As a general rule of thumb, parameters that describe the shape of the deformation are more influenced by corneal properties, whereas parameters that describe the vertical displacement of the cornea to the air pulse are more influenced by IOP. Two parameters that have been shown to be strongly related to biomechanical properties are DAratio2mm and integrated Radius:
Structural and Material Stiffness Once parameters that are more influenced by biomechanical properties and less by IOP are derived, these two main factors can be further differentiated by inverse FEM simulations. Based on these simulations and analytical models, the geometrical bending stiffness can be simply determined by measuring the force that is needed to deform the cornea by a certain amount. Related to the ImTopScanner this bending stiffness could then be determined based on the force on the corneal surface induced by the air pulse, the intraocular pressure and the vertical displacement of the cornea. The Stiffness Parameter has been shown to be highly sensitive in regards of keratoconus detection(1,2). Material stiffness reflects only the intrinsic material properties determined by the structure of the tissue and not influenced by thickness or shape. Numerical simulations are required to obtain material stiffness from the high-speed videos of an OCT or Scheimpflug device. This has been achieved in cooperation with the Biomedical Engineering at University of Liverpool by deriving a stress-strain index that represents the whole stress-strain behaviour of the cornea. This curves have been shown to be mainly independent from IOP and corneal thickness as expected(3). Corneal crosslinking is a key treatment for keratoconus, where mainly the material stiffness increases by creating additional crosslinks within the tissue. When applying this concept to OCT technology, this method has the potential to optimize corneal-crosslinking procedures in order to maximize the stiffening effect of the cornea. (1) Vinciguerra R et al.: “Detection of Keratoconus with a New Biomechanical Index.” Journal of Refractive Surgery 32 (12), 2016: 803-810
(2)Roberts et al.: “Introduction of Two Novel Stiffness Parameters and Interpretation of Air Puff Induced Biomechanical Deformation Response Parameters with a Dynamic Scheimpflug Analyzer.” Journal of Refractive Surgery 33(4), 2017: 266-273 (3)Eliasy A, Chen KJ, Vinciguerra R, Lopes BT, Abass A, Vinciguerra P, Ambrósio R Jr, Roberts CJ, Elsheikh A. Determination of Corneal Biomechanical Behavior in-vivo for Healthy Eyes Using CorVis ST Tonometry: Stress-Strain Index. Front Bioeng Biotechnol. 2019;7:105.
0 Comments
by Enrique Gambra, CTO at 2EyesVision The most common image we have of an ophthalmology device is probably a relatively large desktop instrument with a chin and a front rest for patient stability and a joystick to align the patient with the system. However, in the last years there has been a considerable development of new instruments enabled by new technologies and driven by two main market needs: telemedicine, which has been accelerated by COVID-19 pandemics, and access to rural areas or emergency situations. In both cases, there is a clear need in the clinical practice of new devices that are portable, low-cost and easy-to-use to evaluate vision. A basic set would contain a phoropter or autorefractor, a portable slit lamp, a fundus camera and a tonometer, but the current offer of portable instruments also include corneal topographers, OCTs, wavefront aberrometers or electroretinogram devices. The benefits of portable devices can also be applied to regular office practice. This type of devices usually has a lower cost, require smaller space in the clinic, and many of them are handheld, what can facilitate use in patients with reduced mobility. Other approaches to portable devices include head-mounted devices and technologies based on mobile phones or tablets.
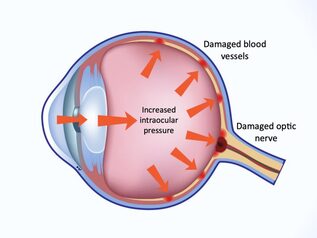
On the other hand, portability introduces a higher risk of damaging the unit, and alignment becomes an even more critical feature. Manufacturers must therefore concentrate in delivering a very robust product with special emphasis on algorithms that help the clinician in achieving the proper alignment. Within IMCUSTOMEYE project, we are developing new technologies and devices for the Ophthalmic and Optometric practice. The first of the technologies is based on Optical Coherence Tomography (OCT) and will evaluate biomechanical properties of the cornea to diagnose corneal abnormalities. This technology is highly sophisticated, with stronger requirements on eye alignment stability, so the final product is expected to be a desktop device. The second technology attempts to detect the presence of corneal abnormalities and refer the patient to the ophthalmologist. This device is expected to be portable to facilitate its use in any environment for screening purposes. by Soledad Aguilar Munoa, Glaucoma Surgical Trials Fellow at Moorfields Eye Hospital Glaucoma is the leading cause of irreversible blindness worldwide, with an estimate of 65.5 million people suffering from primary open-angle glaucoma in 2020. Despite the multifactorial nature of the disease, to date, intraocular pressure (IOP) is the only modifiable risk factor. For this reason, the accuracy of IOP measurement is crucial in the screening, diagnosis, and management of glaucoma. The clinical methods for determining IOP are subject to multiple sources of error, which result in clinically relevant inaccuracies. In particular, the biomechanical properties of the cornea have shown to be an important source of measurement error that could account for major deviations from the true IOP.
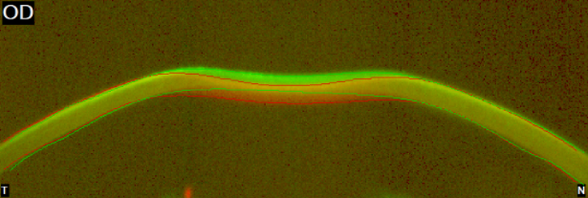
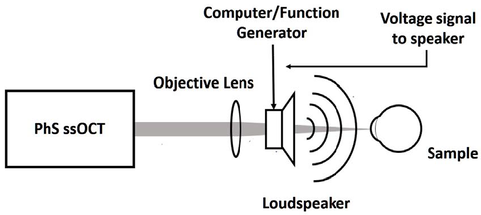
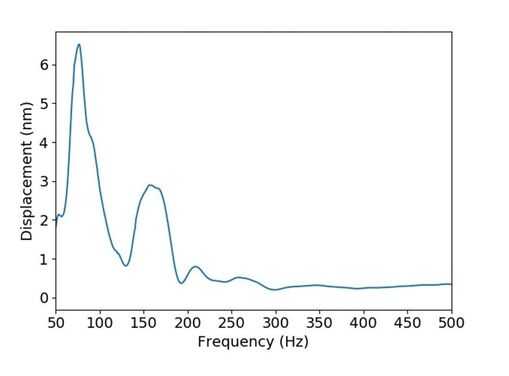
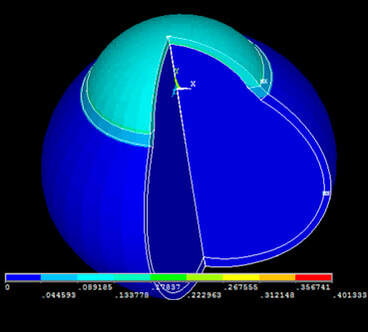
Biomechanics is the application of mechanical engineering principles to living organisms. Viscosity is the quantity that describes a fluid's resistance to flow. Elasticity is the property of solid materials to return to their original shape and size after the forces deforming them have been removed. The cornea exhibits a viscoelastic behaviour. This means that it shares characteristics with viscous and elastic materials. Several devices have attempted to measure the biomechanical properties of the cornea in order to correct IOP measurements. Of those, the Ocular Response Analyzer (Reichert, Inc., Depew, NY) and the Corvis ST (OCULUS Optikgeräte GmbH, Wetzlar, Germany) are the most widely used. However, as IOP measurements are influenced by biomechanics, the measurement of corneal biomechanics in vivo is strongly influenced by IOP, and uncoupling one parameter from the other proves highly challenging. The devices designed within the scope of IMCUSTOMEYE project will aim at performing more accurate measurements of intraocular pressure and corneal biomechanical properties and will hopefully contribute to better glaucoma care and increased knowledge about the nature of the disease. by Andrew Nolan, Postdoctoral Researcher at National University of Ireland Galway It has been noted in previous blog posts that an understanding of the biomechanics of the cornea is fundamental in the detection and treatment of corneal abnormalities such as keratoconus or corneal ectasia. The typical approach to measuring the mechanical properties of an object is to stimulate the object with some external force and measure the response of the object. Since the 1950’s, Goldmann tonometry has been the gold-standard in the measurement of intra-ocular pressure. This involves applying an air puff to the eye and measuring force required to flatten, or applanate, the cornea. Analysing high frequency OCT images of the deformation of the cornea in response to the applied air puff, information about corneal biomechanics, corneal stiffness and viscoelasticity, can be obtained. A clinical device capable of providing such corneal biomechanical information, based on two trusted and well-established technologies, air-puff tonometry and OCT, would be of great benefit to clinicians in diagnosis and treatment planning. In parallel to this, much can be learned about the mechanical properties of an object by observing the frequencies at which it responds to a stimulus. In work being carried out here in NUIG, in collaboration with our partners in CSIC and 2EyesVision, a system is being developed to stimulate the cornea over a range of frequencies using sound excitation. By exciting the cornea over an appropriate range of frequencies using a speaker and measuring the response of the cornea using OCT or other interferometric systems, a full picture of the frequency response of the cornea can be formed. Based on simulations carried out by our colleagues in the University of Liverpool, a possible biomarker has been isolated which would relate corneal frequency response to corneal abnormality. Developing our stimulation and measurement technologies further, we hope to produce a hand held, low cost screening device for corneal abnormality. This device will provide a valuable tool for community screening of diseases such as keratoconus which can cause such difficulty if not detected early. by Alejandra Consejo, Postdoc Researcher & Assistant Professor, Polish Academy of Sciences IMCUSTOMEYE will join Optical Coherence Tomography (OCT) with dynamic imaging of the cornea to assess its biomechanical properties and bring this technology into the clinic with portable instrumentation. OCT is a non-invasive imaging test. ‘Optical’ refers to light. ‘Coherence’ refers to a property of light, and ‘Tomography’ is imaging by sections (slides). OCT uses low-coherence light to capture micrometer-resolution, two- and three-dimensional images from within optical scattering media (e.g., biological tissue). Optical coherence tomography is one of a class of optical tomographic techniques. Commercially available OCT systems are employed in diverse applications, including art conservation and diagnostic medicine, notably in ophthalmology. The advent of OCT imaging has changed the way ophthalmologists image the ocular surface and anterior segment of the eye. Its ability to obtain a dynamic, high, and ultra-high resolution, cross-sectional images of the ocular surface, and anterior segment in a non-invasive and rapid manner allows for ease of use. The Physical Optics and Biophotonics Group at the Polish Academy of Sciences, lead by Prof. Maciej Wojtkowski, is a pioneer in developing new, top-class imaging systems and specialized in Optical Coherence Tomography technology. Figures 1 and 2 are examples of OCT developments performed by prof. Wojtkowski’s team and collaborators. Figure 1. Three-dimensional cutaway view of the human cornea acquired in vivo. Acquired from ‘In vivo imaging of the human cornea with high-speed and high-resolution Fourier-domain full-field optical coherence tomography’ (2020). This research work was developed by Prof. Wojtkowski’s team, and it is available in full here. Figure 2. Figure adapted from ‘Assessment of the influence of viscoelasticity of cornea in animal ex vivo model using air-puff optical coherence tomography and corneal hysteresis’ (2019), co-authored by Dr. Karnowski and Prof. Wojtkowski. Available in full here. This work uses enucleated porcine corneas to demonstrate the usefulness of imaging the cornea using OCT, while mechanically stimulating it with an air pulse, to gain information on corneal viscoelasticity.
by Ahmed Elsheikh, Professor of Biomaterial Mechanics, University of LiverpoolThe cornea plays an important role in allowing us to form clear images of the world. It is responsible for two thirds of the refractive power of the eye, or its ability to focus light on the retina. This important function is only possible when the cornea maintains a particular curved shape, which depends on a fine equilibrium between the eye’s internal fluid pressure and the cornea’s mechanical resistance or biomechanics.
With diseases, such as keratoconus, the cornea’s biomechanics deteriorates causing bulging, loss of the tissue’s regular shape and loss of clear vision. The ability to measure corneal biomechanics is of great clinical importance. There are several processes and surgical procedures that either interact or interfere with corneal biomechanics, and in these cases, knowledge of biomechanics is essential for their customisation for individual patients’ needs. For example, the ability to characterise the deterioration of corneal biomechanics in keratoconic eyes would enable customisation of a treatment regime called collagen cross-linking that can stiffen the tissue to its natural levels. Another example is in refractive surgeries such as LASIK and SMILE. These surgeries involve removing a tissue layer in order to re-shape the cornea’s front surface. With tissue loss, cornea’s stiffness reduces, allowing it to deform more under the eye’s internal pressure. In these applications, knowledge of corneal biomechanics would allow the accurate prediction of post-surgery corneal shape and hence better selection of surgery parameters. Other applications include cataract surgeries where a peripheral incision is made in the cornea to enable removing the natural crystalline lens and introduction of the artificial intraocular lens in its place. This incision changes corneal biomechanics leading to changes in its geometry. The ability to measure corneal biomechanics in vivo has been a major challenge. While we knew from ex vivo laboratory experiments that the biomechanics change with age and diseases (such as keratoconus, diabetes and glaucoma), we have not been able to measure the tissue’s biomechanical properties in vivo. Our IMCUSTOMEYE project is intended to address this challenge through the development of medical devices that can estimate corneal stiffness and viscoelasticity (the most important corneal biomechanical properties) in vivo. Initial results indicate the robustness of our new technologies and their suitability for clinical application within a few years of project end. Our studies will go beyond the measurement of corneal stiffness and viscoelasticity to their implementation to customise various clinical processes and procedures. by Susana Marcos, CSIC, IMCUSTOMEYE Project Coordinator IMCUSTOMEYE is an European Consortium of academic experts in ocular imaging and ocular biomechanics, eye clinics and companies, delivering a new technology to improve ocular diagnostics based on biomechanical biomarkers and personalized treatment.
The cornea is the most external lens in the eye. Along with the crystalline lens, it projects the images of the outside world onto the retina. The cornea is a transparent dome and its structural integrity relies on a finely interleaved collagen fibers. The regular shape of the cornea is therefore the result of its biomechanical rigidity. However, the cornea is not a piece of plastic, and different corneas may respond differently to mechanical stimuli. In several pathologies, such as keratoconus, the corneal weakens locally, resulting in corneal bulging and vision distortion. Keratoconus affects 1% of the population and treatment requires implating a supporting structure inside the cornea (intracorneal ring segments) or stiffening the cornea instilling a dye and irradiating with light (a technique called keratoconus). There are other ocular conditions in which the cornea is reshaped or surgically open. These conditions are highly prevalent, such as myopia that affects 30% of the population in western countries and 90% in some Asian populations; presbyopia, the age-related loss of dynami focusing capacity, which affecs 100% of people older than 45; and cataract, the loss of transparency with affects 50% of the population older than 65. In corneal refractive surgery, used to correct eye’s refractive errors a laser is used to evaporate or remove corneal tissue to sculpt the cornea into a different shape. Alternatively, new techniques are being developed where biomaterials or tissue is implanted in the cornea to correct presbyopia. In cataract surgery, an intraocular lens is implanted through an incision that needs to be made in the cornea. While all these treatments rely to a larger or lesser extent on the mechanical response of the cornea, today there is no clinical instrument that either detects corneal mechanical abnormalities, or can help in predicting the mechanical response to surgery. IMCUSTOMEYE, a Project funded by the European Commission Horizon 2020 program addresses this unmet medical need. IMCUSTOMEYE has gathered a highly internatonally reputed multidisciplinary group of experts in academia, industry and clinic to deliver and demonstrate a new clinical instrument which will put Europe in the forefront of personalized diagnostics in opthalmology. The Project is Coordinated by VioBio Lab at the National Research Council (CSIC) in Spain, a group that has pioneered multiple optical imaging eye diagnostics and includes world leaders in biomedical optics and photonics at the Institute of Chemistry and Physics, of the Polish Academy of Sciences and National University of Ireland, Galway, and internationally reputed engineers experts in corneal biomechanics from the University of Liverpool. International companies, selected for their unique technical expertise in the ophthalmic industry and strategic position in the field. 2EyesVision in Spain,which has launched headmounted diagnostic tolos to help in intraocular lens selection in cataract surgery. Oculus in Germany , with a large portfolio of clinical instruments, including the Corvis corneal deformation imaging Optimeyes in Switzerland, with the only software worldwide to guide opthalmic surgical procedures. And IROC in Switzerland, and expert in bridging technology from the lab into a product in the ophthalmic market will ensure an efficient translation of the front-end laboratory designs and prototypes into a viable clinical instrument. IMCUSTOMEYE’s team also includes most acclaimed ophthalmology clinics, Moorfields Eye Hospital and Instituto Oftalmologico Fernandez Vega, both with flows of thousands of patients day and high clinical standards. The pilot clinical studies with the developed intrumentation will proof the technology and the expected benefits for patients. |
Proudly powered by Weebly